Naloxone can save lives, but employers need a plan
Prolonged use of prescription opioids for chronic pain can lead to addiction, which can result in overdose. Workplaces are not immune to these tragedies. While the drug naloxone can temporarily stop many of the life-threatening effects of opioid overdose, employers need to be informed before they implement its use.
Naloxone use considerations
Employers that want to make naloxone (also known as Narcan) available in the workplace should consider a naloxone use program. This program is often part of a more comprehensive workplace program on opioid awareness and misuse prevention. When deciding whether such a program is needed or feasible, employers should consider the following:
- State laws. Does your state allow the administration of naloxone by non-licensed providers, such as first aid team members?
- Liability and legality. What liability and legal considerations should be addressed? Does your state’s Good Samaritan law cover emergency naloxone administration?
- Staff. Do you have staff willing to be trained and willing to provide naloxone?
- Need and geographic location. Is there a foreseeable need? Has your workplace experienced an opioid overdose or found evidence of opioid drug use on site (such as finding drugs, needles, or other paraphernalia)? Are the risks of opioid overdose greater in your industry? Are the risks greater in your geographic location?
- Assistance from EMS. How quickly can professional emergency response personnel access your workplace?
- Pre-existing interventions. Does your workplace offer other first aid or emergency response interventions (first aid kits, AEDs, trained first aid providers)? Can naloxone be added?
- Visiting public. Does your workplace have frequent visitors, clients, contractors, patients, or other members of the public that may be at increased risk of opioid overdose?
Naloxone program, policies, and procedures
Safety professionals need to work with company leadership to develop effective policies and procedures for a naloxone use program. Involving a workplace safety committee and worker representatives is also crucial in understanding the need for such a program. When establishing a program, include the following:
- Conduct a risk assessment
- Evaluate worker and visitor risk of overdose by reviewing near-miss reports and injury/illness logs. Search state and local health department websites to determine opioid hot spots and areas of concern.
- Identify staff willing to take training and provide naloxone, which may be different than those willing to perform CPR and utilize an AED.
- Consult with EMS and local healthcare professionals who treat opioid use disorders in your area.
- Consider liability
- Discuss with your insurance carrier any liability and other legal issues. Keep in mind that all 50 states have naloxone access laws designed to make the distribution and use of this medication more available.
- Understand your state’s Good Samaritan Laws, which provide immunity for those who act in good faith to seek medical care.
- Manage records
- Establish formal procedures for documenting incidents and managing those records.
- Include a process for safeguarding the privacy of the affected individual.
- Maintain records related to staff roles and training.
- Define staff roles
- Define roles and responsibilities for individuals designated to respond to a suspected overdose.
- Amend existing first aid or emergency response policies and procedures to include the addition of naloxone use.
- Train staff
- Train staff to recognize the symptoms of a possible opioid overdose. Call 9-1-1 to seek immediate medical assistance.
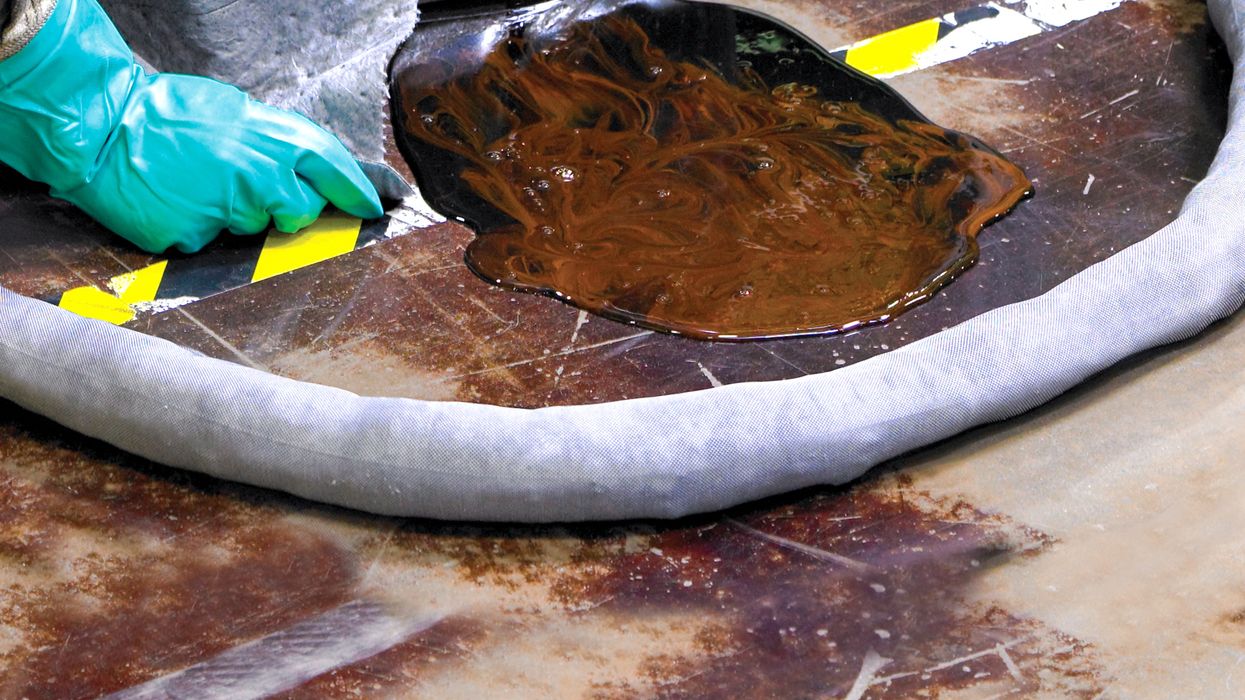
- Know the dangers of exposure to drug powders/residue. Assess the incident scene before entering (and know when not to enter).
- Use personal protective equipment during all responses.
- Customize training for the administration of intranasal or injectable naloxone and recognize when additional doses are needed.
- Address any symptoms that may arise during response. Use additional first aid or CPR as needed.
- Prepare for possible exposure to blood, needles or other sharps (provide bloodborne pathogen training and consider hepatitis B vaccination).
- Schedule refresher training annually; can be combined with other first aid/CPR training and certifications.
- Purchase naloxone
- Choose nasal sprays or injectable forms that can be delivered with an auto-injector, pre-filled syringe, or a standard syringe/needle. Research shows that people trained on intranasal spray reported higher confidence in administration.
- Stock a minimum of two doses. In some cases, one dose of naloxone is inadequate to reverse an overdose.
- Consider the time needed to replace supplies when determining the number of doses to stock.
- Store naloxone
- Follow manufacturer instructions.
- Store in locations that allow immediate access.
- Note the expiration date for timely replacement.
- Acquire and maintain adequate PPE
- Store personal protective equipment (PPE) close to the naloxone for quick response.
- Include fentanyl-resistant nitrile gloves, rescue mask, face shield, or bag valve mask, along with sharps disposal containers (if injectable naloxone is used).
- Develop follow-up care planning
- Work with healthcare providers to develop a plan for immediate care, as well as ongoing support for any worker who has overdosed.
- Include emergency assistance and support for naloxone-trained staff and/or bystanders if necessary.
- Maintain your program
- Re-evaluate and update your program on a periodic basis.
- Include any new medical and emergency response guidance as it becomes available.
In 2022, over 82,136 people died of a drug overdose involving opioids (including heroin, OxyContin, Vicodin, fentanyl, etc.). Until 2023, naloxone was available only by prescription. To increase its accessibility, many states issued standing orders or third-party prescriptions, which allow pharmacists to dispense naloxone without a prescription. Employers need to understand the risks and considerations before deciding whether to allow naloxone use in the workplace.
Key to remember: While naloxone can reverse the effects of an opioid overdose at work, employers should consider the risks and their responsibilities before purchasing it.