Industrial hygiene is the science devoted to the anticipation, recognition, evaluation, and control of the environmental factors or stresses in the workplace that may cause illness, injury, impaired health or well-being, or significant discomfort for a worker.
Hearing conservation and noise
- OSHA requires employers to monitor noise in the workplace, and to implement engineering or administrative controls to control excessive noise. If controls are not enough, employers must have a hearing conservation program.
The Occupational Safety and Health Administration (OSHA) requires employers to determine if workers are exposed to excessive noise in the workplace. If so, the employer must implement feasible engineering or administrative controls to eliminate or reduce hazardous levels of noise. Where controls are not sufficient, employers must implement an effective hearing conservation program.
OSHA’s occupational noise exposure standard at 1910.95 is designed to protect general industry employees, such as those working in the manufacturing, utilities, and service sectors. It does not cover the construction or the oil and gas well drilling and servicing industries.
Summary of requirements
- Employers must implement an effective hearing conservation program if employee noise exposure is equal to or greater than an eight-hour TWA of 85 decibels.
- Employees must be trained on the hazards of excessive noise, be hearing tested when needed, and use hearing protectors if necessary.
Employers are required to:
- Administer a continuing, effective hearing conservation program IF employee noise exposures equal or exceed an eight-hour time-weighted average sound level (TWA) of 85 decibels measured on the A scale (slow response); OR equivalently, a dose of 50 percent.
- Institute a training program for all employees who are exposed to noise at or above an eight-hour time-weighted average of 85 decibels, AND ensure employee participation in such program.
- Make copies of 1910.95 available to affected employees or their representatives and also post a copy in the workplace.
- Use feasible administrative or engineering controls where needed.
- Establish and maintain an audiometric testing program by making audiometric testing available to all employees whose exposures equal or exceed an eight-hour time-weighted average of 85 decibels.
- Develop and implement a monitoring program if information indicates that any employee’s exposure may equal or exceed an eight-hour time-weighted average of 85 decibels.
- Maintain an accurate record of all employee exposure measurements required.
- Make hearing protectors available, at no cost, to all employees exposed to an eight-hour time-weighted average of 85 decibels or greater.
- Evaluate hearing protector attenuation for the specific noise environments in which the protector will be used.
How noise works
- Exposure to high levels of noise in the workplace can lead to hearing loss, as well as increased muscle tension, quickened pulse and increased blood pressure. This affects safety and productivity.
- Noise generally is classified as continuous, intermittent, or impact.
Noise is a by-product of many industrial processes and exposure to high levels of noise can cause hearing loss. It can also cause stress on other parts of the body, resulting in increased muscle tension, a quickened pulse rate, and increased blood pressure. Workers exposed to excessive noise sometimes experience nervousness, sleeplessness, and extreme fatigue, all of which can affect productivity, quality, and safety.
Noise can cause temporary or permanent hearing loss. Temporary hearing loss results from short-term exposures to noise, with normal hearing returning after a period of rest. Prolonged exposure to high noise levels over a period of time gradually causes permanent damage, which equally affects both ears.
Noise can be broken down into three general classifications:
- Continuous — wide-band noise of about the same constant level of amplitude, frequency content, and duration (such as is found with engines and fans). Sounds repeated more than once each second are considered constant or steady.
- Intermittent — exposure to wide-band noise several times during the work shift (such as is found with power tools and discharges from steam or air-pressure relief valves).
- Impact — temporary pulsing or a sharp burst of sound, usually less than a half second in duration, which is not repeated more than once each second (such as is found with power punch presses and jack hammers).
Effects of excessive exposure
- Noise affects hearing by damaging the sensitive hair cells of the inner ear. Depending on length of time and level of exposure, this effect may be temporary or it can be permanent.
People differ in their sensitivity to sound, and there’s no way to determine who is most at risk for hearing damage. Factors such as sound pressure, frequency, and length of exposure all play roles in determining whether what a person hears is harmful or just annoying.
When noise is too loud, it can damage the sensitive hair cells of the inner ear. As the number of damaged hair cells increases, the brain receives fewer impulses to interpret as sound. While a single exposure to loud noise can damage hair cells, it probably won’t destroy them. The person may experience ringing in the ears and some sounds may be muffled, but the hair cells will recover and so will hearing. This is called a temporary threshold shift. But without proper hearing protection, repeated exposures to loud noise can damage hair cells to the point that they won’t recover. Because the damage is severe, it results in a permanent threshold shift, and no treatment will restore it.
In its early stages, when hearing loss is above 2,000 hertz, it affects the ability to understand or discriminate speech. As it progresses to the lower frequencies, it begins to affect the ability to hear sounds in general. The three main types of hearing loss are conductive, sensorineural, or a combination of the two.
The effects of noise can be simplified into three general categories:
- Primary effects: Noise-induced temporary threshold shift, noise-induced permanent threshold shift, acoustic trauma, and tinnitus.
- Effects on communication and performance: Isolation, annoyance, difficulty concentrating, absenteeism, and accidents.
- Other effects: Stress, muscle tension, ulcers, increased blood pressure, and hypertension.
Ultrasonics
- Though inaudible to the human ear, ultrasound may still affect hearing.
Ultrasound is high-frequency sound that is inaudible to, or cannot be heard by, the human ear. However, it may still affect hearing and produce other health effects. Factors to consider regarding ultrasonics include:
- The upper frequency of audibility of the human ear is approximately 15–20 kilohertz.
- This is not a set limit and some individuals may have higher or lower (usually lower) limits.
- The frequency limit normally declines with age.
- Most of the audible noise associated with ultrasonic sources, such as ultrasonic welders or ultrasonic cleaners, consists of subharmonics of the machine’s major ultrasonic frequencies.
- Example: Many ultrasonic welders have a fundamental operating frequency of 20 kilohertz, a sound that is at the upper frequency of audibility of the human ear. However, a good deal of noise may be present at 10 kilohertz, the first subharmonic frequency of the 20 kilohertz operating frequency, and is therefore audible to most persons.
Evaluating noise exposure
- Employers must determine the level of noise their employees are exposed to in the workplace in order to determine which control methods are needed to protect worker safety.
The first step toward solving any noise problem is to define it. To understand what requirements must be implemented according to the Occupational Safety and Health Administration (OSHA)’s noise standard, it is necessary to determine exposure levels.
When evaluating which employees are potentially covered by OSHA’s standard, keep in mind that the rule applies to employees with even one day of exposure to noise levels at or above 85 decibels on an eight-hour time weighted average (TWA). Such employees must therefore be included in the company’s hearing conservation program. For example, if an employee visits a particular facility only a few times per year, but is exposed to noise levels at or above 85 decibels on a TWA, that employee would be covered by the standard.
Employees who have not been exposed to noise levels equal to or exceeding 85 decibels (as an eight-hour TWA) for an entire year following their last annual audiogram may be removed from the hearing conservation program.
Indications of a problem
- Subjective responses, such as workers having to shout to be heard in conversation, may be a warning that workplace noise is at an unacceptable level.
- Lower levels of noise exposure may actually be more dangerous, because the worker may perceive it as not loud enough to require hearing protection.
There are various factors that indicate when noise is a problem in the workplace. While people react differently to noise, subjective responses should not be ignored because they may provide warnings that noise may be at unacceptable levels.
- Noisy conditions can make normal conversation difficult. When noise levels are:
- Above 80 decibels, people have to speak very loudly.
- Between 85 and 90 decibels, people have to shout.
- Greater than 95 decibels, people have to move close together to hear each other at all.
- High noise levels can cause adverse reactions or behaviors.
Lower levels of noise exposure may actually be riskier than higher levels. Exposures below 95 decibels may be annoying, but don’t seem loud enough for hearing protection — though cumulative exposure can lead to hearing loss. Noise levels above 100 decibels, however, are uncomfortable and the discomfort serves as a reminder to wear hearing protection.
Sometimes, overexposure to loud noise can trigger ringing or other sounds in the ears. This is called tinnitus. While tinnitus may be a symptom of damaged hearing, it can also be caused by infections, medications, and impacted ear wax. The only way to know for sure if noise has damaged a person’s hearing is to have a hearing examination by a certified audiometric technician, audiologist, otolaryngologist, or physician.
Don’t forget that exposure to loud noise doesn’t occur in just the workplace. Off the job, employees can be exposed to noise from firearms, motorcycles, snowmobiles, power tools, lawn mowers and snow blowers, and loud music, often from headphones/earbuds with personal media devices.
Noise surveys
- Employers should engage a trained individual to conduct a walk-around sound survey of their workplaces.
There’s only one way to know if noise has reached a dangerous level — by having a trained person conduct a noise survey. Anyone trained to use a sound level meter and a dosimeter and evaluate the data should be able to perform the survey.
The walk-around survey will screen for noise exposures and determine if additional monitoring is necessary. When screening for noise exposures, sound-level meter measurements and estimates of the duration of exposure are sufficient. The resulting spot readings can be used to determine the need for a more complete evaluation. Survey steps to follow include:
- Touring the facility and developing a detailed understanding of facility operations and potential noise sources. Employers should take the tour with someone who is familiar with plant operations and maintenance requirements. Notes should be taken on a diagram of the floor plan if possible. The employer will need to look for indications that noise may be a problem.
- Using a sound level meter to take spot readings of operations that are questionable. It may be useful to mark the sound levels on a diagram of the floor plan. Notes should be taken regarding what equipment is on or off.
- Estimating exposures by identifying employees and their locations and estimating the length of time they spend in different areas or how long they operate particular equipment or tools.
If the results of the walk-around survey indicate time-weighted average (TWA) exposures of 80 decibels or more, additional noise monitoring should be performed. Employers should take into account the accuracy of the sound level meter when making this estimation. For example, a Type 2 sound level meter has an accuracy of plus or minus 2 decibels.
Work shift sampling
- If a walk-around sound survey indicates excessive noise levels, employers will need to implement additional monitoring.
When the results of the walk-around survey indicate that noise levels may exceed those outlined in the Occupational Safety and Health Administration (OSHA)’s Occupational Noise Exposure standard at 1910.95, additional monitoring is necessary. Sample the noise exposures of representative employees from each job classification that may be potentially overexposed.
Use a dosimeter with a threshold of 80 decibels (A-weighted sound pressure level) and 90 decibels to measure noise exposures. Most modern dosimeters use simultaneous 80 and 90 decibel thresholds.
- A dosimeter with a threshold of 80 decibels is used to measure the noise dose of those employees identified during the walk-around survey as having noise exposures that are in compliance with Table G-16 of OSHA’s noise standard 1910.95, but whose exposure may exceed the levels specified in Table G-16a [1910.95 Appendix A: Noise Exposure Computation]. In other words, the 80-decibels threshold is used to determine compliance with the 85 decibels time-weighted average (TWA) action level under OSHA’s noise standard.
- The dosimeter with a threshold of 90 decibels is used to measure the noise dose of those employees identified during the walk-around survey as having potential noise exposures that exceed the sound levels in Table G-16. In other words, the 90 decibels threshold is used to determine compliance with the permissible exposure limit (PEL).
As a minimum, sampling should be conducted for a length of time necessary to establish whether exposures are above the limits permitted by Table G-16 or Table G-16a. Instrument accuracy must be taken into account. Employers should consider the following with respect to the monitoring results:
- TWA exposures at or above the action level of 85 decibels require a hearing conservation program (results obtained from the 80 decibels threshold).
- TWA exposures exceeding the PEL (Table G-16) require feasible engineering or administrative controls to be implemented (results obtained from the 90 decibels threshold).
Measuring sound
- The instruments most commonly used to measure sound are the sound level meter, the dosimeter, and the octave-band analyzer.
Instruments generally used to measure sound include:
- Sound level meter
- Dosimeter
- Octave-band analyzer
Important factors to consider when dealing with these instruments are instrument settings, calibration, and effects of the environment on instrumentation.
Sound level meter
There are various factors that may indicate noise is a problem in the workplace. While people react differently to noise, subjective responses should not be ignored because they may provide warnings that noise may be at unacceptable levels. A sound level meter (SLM) is the basic instrument for investigating noise levels.
Sound level meters can be used to:
- Spot-check noise dosimeter performance.
- Determine an employee’s noise dose whenever use of a noise dosimeter is unavailable or inappropriate.
- Identify and evaluate individual noise sources for abatement purposes.
- Aid in determining the feasibility of engineering controls for individual noise sources.
- Evaluate hearing protectors.
Factors to consider with the use of a SLM include:
- When evaluating employee exposures, the microphone should be placed in the hearing zone of the employee being monitored.
- Sound level readings in a non-reverberant environment should be taken in accordance with the manufacturer’s instructions.
- Special considerations may be involved with the use and care of a sound level meter.
Dosimeter
Like a sound level meter, a noise dosimeter can also measure sound levels. However, the dosimeter is actually worn by the employee in order to determine the personal noise dose during the work shift or sampling period. Dosimeters can be used to:
- Take compliance measurements according to the Occupational Safety and Health Administration (OSHA)’s noise standard.
- Measure the employee’s exposure to noise and automatically compute the necessary noise dose calculations.
Factors to consider with the use of a dosimeter include:
- The microphone must be placed in the employee’s hearing zone. OSHA defines the hearing zone as a sphere with a two-foot diameter surrounding the head.
- Specific instrument settings must be selected for the dosimeter.
- Special considerations may be involved with the use and care of a dosimeter.
Octave-band analyzers
Octave-band analyzers are sound level meters that can be used to:
- Help determine the adequacy of various types of frequency-dependent noise controls.
- Select hearing protectors because they can measure the amount of attenuation (how much a sound is weakened) offered by the protectors in the octave bands responsible for most of the sound energy in a given situation.
- Divide noise into its frequency components.
- Some sound level meters may have an octave or one-third octave band filter attached or integrated into the instrument. Usually a Type 1 (precision) sound level meter is used for octave and one-third octave analysis.
- The filters are used to analyze the frequency content of noise. They are also valuable for the calibration of audiometers and to determine the adequacy of various types of noise control.
Frequency components may include:
- Most octave-band filter sets provide filters with the following center frequencies: 31.5, 63, 125, 250, 500, 1,000, 2,000, 4,000, 8,000, and 16,000 hertz.
- For a more detailed analysis, the spectrum is sometimes measured in one-third octave bands.
- The special signature of any given noise can be obtained by taking sound level meter readings at each of the center frequency bands. The results may indicate octave bands that contain the majority of the total sound power being radiated.
Controlling workplace noise
- Once noise levels exceed an eight-hour TWA of 90 decibels, it is time for employers to implement additional controls.
Once an employer becomes aware of a noise problem in the workplace — usually meaning employee exposure levels exceeding an eight-hour time-weighted average (TWA) of 90 decibels — the next step is to decide how to combat the problem. Engineering and administrative controls are essential to putting up an effective fight against workplace noise.
Engineering controls
- Engineering controls are the best way to control noise, when such controls are effective, practical and affordable.
Workplace safety and health specialists agree that engineering controls are the best way to control noise. That’s true if the engineering control is effective, practical, and affordable. Replacing a noisy machine with a quiet one, modifying it to make it quieter, or changing the sound path so that the noise never reaches the listener are all examples of engineering controls.
- Replacement. An old, noisy electric hand drill can be easily replaced with a newer, quieter one, but replacing a large, noisy chipper/shredder may not be practical.
- Enclose the offending equipment. Creative solutions may also be effective ones. Construction workers were using a concrete mixer to de-grease metal parts by tumbling them in sawdust — effective, but noisy. To reduce the noise level to below 85 decibels, the employer built an enclosure around the mixer with two-by-fours and acoustic sound board, sealing the access door with polyurethane foam. The cost was minimal and the design was effective; it lowered noise levels to 78 decibels.
- Increase the distance. Doubling the distance between the worker and the sound source can decrease the sound pressure level by six decibels. For example, a hazardous 96-decibel noise source at five feet is a safe 84 decibels at 20 feet.
- Reduce the impact. Reducing the height that materials collected in bins and boxes will drop can quiet a noisy process. Employers might consider lining containers with damping materials such as plastic or rubber to keep them quiet.
Applying practical engineering controls to a noise problem can be challenging because there may not be ready-to-order solutions. To find a solution, it is important to:
- Understand what’s causing the noise.
- Determine how the noise is reaching the worker.
- Identify the most appropriate point or points at which to control the noise, either at the source, along the sound path, or at the worker.
Administrative and work practice controls
- Administrative and work practice controls emphasize worker activities, such as reducing time spent working in a noisy area or shutting down unused equipment, to help reduce noise exposure.
Unlike engineering controls that prevent hazardous noise from reaching a worker, administrative controls manage workers’ activities to reduce their exposure. Closely related to administrative controls are work practice controls, which emphasize safe practices.
Administrative and work practice controls are usually less expensive than engineering controls because there are no significant capital costs involved in changing or modifying equipment. In some cases, administrative controls can reduce employee exposure to noise and increase productivity by rotating employees through a demanding, noisy task. Work practice controls can also improve performance by emphasizing safe work practices.
Administrative and work practice controls may not be as effective as engineering controls because they don’t control the noise exposure. Noisy machines are still noisy and the exposure is still present. Some controls that can be used to reduce exposure include:
- Reducing the time employees spend working in noisy areas;
- Rotating two or more employees so that each is exposed to noise less than 85 decibels, averaged over an eight-hour day;
- Shutting down noisy equipment when it’s not needed for production;
- Ensuring that employees maintain equipment so that it runs smoothly and quietly;
- Ensuring that employees know how to perform their tasks and operate equipment at safe noise levels;
- Using warning signs to identify work areas where noise exceeds safe levels; and
- Encouraging employees to report noise hazards to supervisors.
If it’s not possible to eliminate or control noise with an engineering control, it may be possible to control it with an administrative control. However, if an administrative control won’t reduce employee exposures to safe levels, an additional noise-control tool may be needed — hearing protectors.
Personal protective equipment: Hearing protection
- When engineering and administrative or work practice controls aren’t enough, employers will need to provide employees with hearing protectors.
- Hearing protectors are usually in the form of either ear plugs or earmuffs.
When workplace noise equals or exceeds 85 decibels, averaged over an eight-hour period, can’t be reduced through engineering, administrative, or work practice controls, employees must be provided with hearing protection at no cost to them. Employees who receive hearing protectors must have the opportunity to select from a variety of types that are compatible with their work tasks. Employees must also be properly fitted and trained to use and care for their hearing protectors.
There are two types of hearing protectors: ear plugs and earmuffs. Both types reduce the pressure of sound that reaches the eardrum and are the next line of defense when noise levels can’t be reduced to safe levels with engineering or administrative controls.
- Expandable foam plugs are made of a formable material designed to expand and conform to the shape of each person’s ear canal. The user rolls the expandable plugs into a thin, crease-free cylinder before inserting into the ear. The plug should be rolled into a smooth tube thin enough so that about half the length will fit easily into the ear canal. Some individuals, especially those with small ear canals, have difficulty rolling typical plugs small enough to make them fit. A few manufacturers now offer a small size expandable plug.
- Pre-molded, reusable plugs are made from silicone, plastic or rubber and are manufactured as either one-size-fits-most or are available in several sizes. Many pre-molded plugs are available in sizes for small, medium or large ear canals.
- Canal caps often resemble earplugs on a flexible plastic or metal band. The earplug tips of a canal cap may be a formable or pre-molded material. Some have headbands that can be worn over the head, behind the neck or under the chin. Newer models have jointed bands increasing the ability to properly seal the earplug.
- Earmuffs come in many models designed to fit most people. They work to block out noise by completely covering the outer ear. Muffs can be “low profile” with small ear cups, or large to hold extra materials for use in extreme noise. Some muffs also include electronic components to help users communicate or to block impulsive noises.
Select the right hearing protection
- Hearing protectors must fit properly, be comfortable, and be easy to wear; otherwise, employees will not wear them correctly or as often as needed.
The best hearing protector is the one that is comfortable and convenient and that will be worn every time a person is in an environment with hazardous noise. Hearing protectors should be selected based not just their attenuation capability but also on comfort, convenience, and compatibility. Employees won’t wear hearing protectors that are uncomfortable or difficult to use or that interfere with their work. To ensure they will wear the protectors, employers should allow employees to choose, with the help of a person trained in fitting hearing protectors, from among a variety of appropriate types and sizes.
Most hearing protectors are labeled with a noise reduction rating (NRR) indicating a protection level in decibels. However, these ratings are not reliable outside of a testing laboratory, which is where they received the rating. The NRR rating tends to overestimate the protection a hearing protector will provide under real-world conditions.
One way to estimate the real-world effectiveness of a hearing protector is to subtract seven decibels from the manufacturer’s NRR as shown below:
Sample NRR Calculation| Noise level to which the worker is exposed, averaged over an eight-hour period | 95 decibels |
| NRR shown on the hearing protector label | 25 decibels |
| Subtract 7 decibels from the NRR | 25 - 7 = 18 |
| Subtract 18 dB from 95 decibels | 95 decibels - 18 dB = 77 decibels |
This hearing protector may be able to reduce the worker’s exposure down to 77 decibels in this 95 decibel environment.
Develop a hearing conservation program
- A hearing conservation program must include monitoring, testing, employee training, provided hearing protection, and recordkeeping.
An effective hearing conservation program can prevent hearing loss, improve employee morale and a general feeling of well-being, increase quality of production, and reduce the incidence of stress-related disease. Employers must administer a continuing, effective hearing conservation program whenever employee noise exposures are at or above an eight-hour time-weighted average (TWA) of 85 decibels or, equivalently, a dose of 50 percent. This is referred to as the action level.
The Occupational Safety and Health Administration (OSHA)’s noise standard (1910.95) contains two noise exposure limit tables. Each table serves a different purpose:
- Table G-16: This table applies to the engineering and administrative controls section, which provides a 90-decibels criterion for an eight-hour TWA permissible exposure limit and is measured using a 90-decibels threshold (i.e., noise below 90 decibels is not integrated into the TWA). This table limits short-term noise exposure to a level not greater than 115 decibels (for up to 15 minutes).
- Table G-16A: This table, presented in Appendix A of 1910.95, provides information (e.g., reference durations) useful for calculating TWA exposures when the work shift noise exposure is composed of two or more periods of noise at different levels. Although this table lists noise levels exceeding 115 decibels, these listings are only intended as aids in calculating TWA exposure levels; the listings for higher noise exposure levels do not imply that these noise levels are acceptable.
Minimum requirements of a hearing conservation program include monitoring, audiometric testing, hearing protection devices, employee training, and recordkeeping.
Monitoring program
- The employer’s monitoring program must be designed to identify all employees who should be included in a company’s hearing conservation program.
Employers must develop and implement a monitoring program whenever information indicates that any employee’s exposure may equal or exceed the action level. The sampling strategy must be designed to identify all employees for inclusion in the hearing conservation program and enable the proper selection of hearing protectors.
The monitoring requirement is performance based, as it allows employers to choose a monitoring method that best suits each individual work situation. Either personal or area monitoring may be used. If there are circumstances that may make area monitoring generally inappropriate, such as high worker mobility, significant variations in sound level or a significant component of impulse noise, then the employer must use representative personal sampling unless it can be shown that area sampling produces equivalent results.
Noise measurements must integrate all continuous, intermittent, and impulsive noise levels from 80 to 130 decibels. Monitoring must be repeated whenever a change in production, process, equipment or controls increases noise exposures to the extent that additional employees may be exposed at or above the action level, or the attenuation provided by hearing protectors used by employees is inadequate.
The employer must notify each employee who is exposed at or above the action level of the results of the monitoring and provide them with an opportunity to observe noise monitoring procedures.
Employee training
- OSHA requires covered employers to train employees on the effects of noise on hearing, the purpose and use of hearing protectors, and the purpose of audiometric testing.
The Occupational Safety and Health Administration (OSHA) requires employers to establish a training program for all employees with noise exposures at or above the action level and ensure employee participation. Training must be repeated annually for each employee in the hearing conservation program and the information must be updated to be consistent with changes in protective equipment and work processes.
The employer must ensure that each employee is informed of:
- The effects of noise on hearing.
- The purpose of hearing protectors, the advantages, disadvantages, and attenuation of various types, and instructions on selection, fitting, use, and care.
- The purpose of audiometric testing and an explanation of test procedures.
Employers must make copies of the OSHA noise standard available to affected employees and post a copy in the workplace. They also are required to provide affected employees with any informational materials pertaining to the standard that are supplied to the employer by OSHA and give OSHA copies of all material relating to the employer’s training and education program (on request).
Documentation
- OSHA requires employers to maintain records of all employee noise exposure measurements, as well as all employee audiometric testing.
The Occupational Safety and Health Administration (OSHA) has specific recordkeeping requirements for noise monitoring and employee testing results.
Employers must maintain an accurate record of all employee exposure measurements. These records must be retained for two years.
The employer must retain all employee audiometric test records. These records must include:
- Name and job classification of the employee.
- Date of the audiogram.
- The examiner’s name.
- Date of the last acoustic or exhaustive calibration of the audiometer.
- Employee’s most recent noise exposure assessment.
Additionally, the employer must maintain accurate records of the background sound pressure level measurements in audiometric test rooms. These records must be maintained for the duration of the affected worker’s employment.
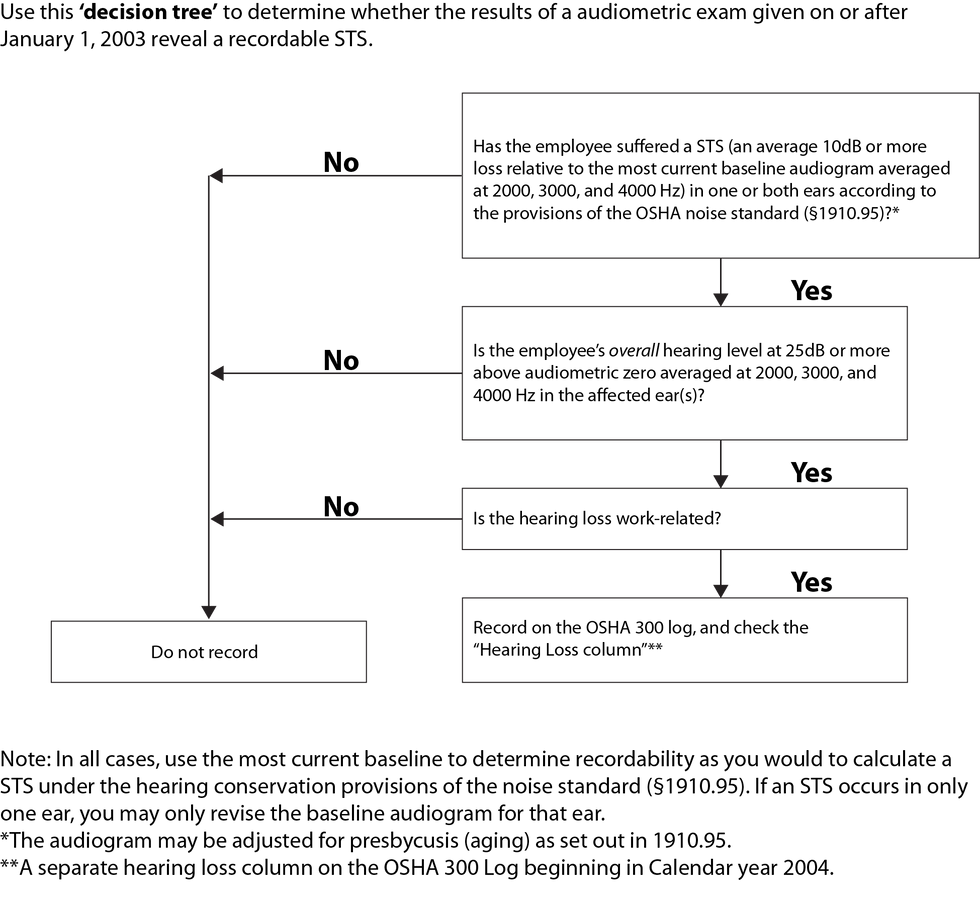
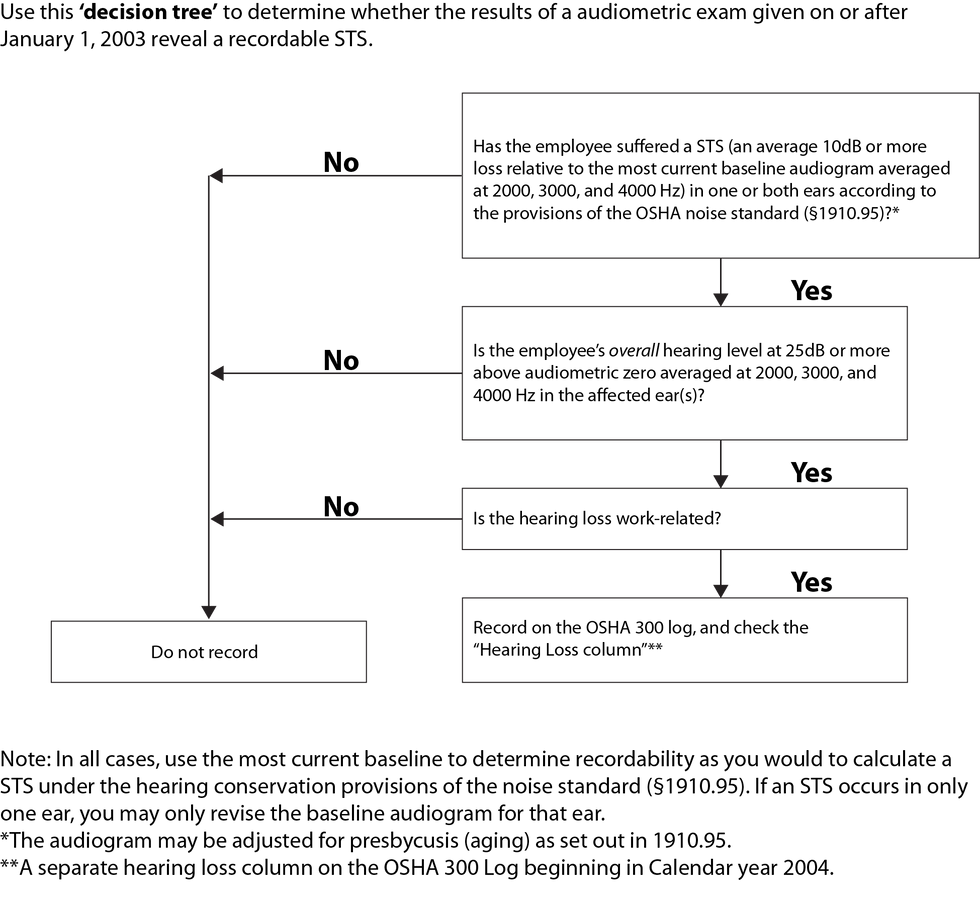
Recording hearing loss on the 300 Log
- Work-related hearing loss above the indicated threshold must be recorded on the OSHA 300 Log.
Noise-induced hearing loss is a serious and irreversible condition. However, it is not the type of occupational injury that typically requires days away from work for recuperation. All work-related hearing losses of 10 decibel shifts that result in a total 25 decibel shift above audiometric zero have to be recorded on the Occupational Safety and Health Administration (OSHA) 300 Log.
Audiometric zero and STS
A standard threshold shift (STS) is a change in hearing threshold, relative to an employee’s baseline audiogram (hearing test), averaging 10 decibels or more at 2,000, 3,000, and 4,000 hertz in one or both ears. If an employee’s audiogram reveals that a work-related STS has occurred in one or both ears, and the total hearing level is 25 decibels or more above audiometric zero in the same ear(s) as the STS, the case is recordable.
If an employee has a recordable STS, employers must document the case by checking the “hearing loss” column on the OSHA 300 Log.
Retesting
Retesting allows employers to exclude false positive results and temporary threshold shifts from the data. If the employee’s hearing is retested within 30 days of the first test, and the retest does not confirm the STS, the employer is not required to record the hearing loss case on the OSHA 300 Log. However, if the retest confirms the STS, the employer must record the hearing loss illness within seven calendar days of the retest.
Hearing loss that occurs with aging
Employers may take into account the hearing loss that occurs as a result of the aging process and retest an employee who has an STS on an audiogram to ensure that the STS is permanent before recording it. When comparing audiogram results, results may be adjusted for the employee’s age when the audiogram was taken using Tables F-1 or F-2, as appropriate, in Appendix F of the Occupational Noise Exposure standard.
Noise dose
Hearing loss is presumed to be work related if the employee is exposed to noise in the workplace at an eight-hour time-weighted average of 85 decibels or greater, or to a total noise dose of 50 percent, as defined in OSHA’s noise exposure standard.
Noise dose is defined as the amount of actual exposure to noise relative to its permissible exposure limit. A dose greater than 100 percent represents exposure above the limit. For hearing loss cases where the employee is not exposed to this level of noise, employers should refer to the rules in 1904.5 to determine if the hearing loss is work-related.
If a physician determines that the hearing loss is not work related or has not been significantly aggravated by occupational noise exposure, the employer is not required to consider the case work related or to record it on the OSHA 300 Log. Some examples are if the hearing loss occurs before the employee is hired, or the hearing loss is unrelated to workplace noise, such as off the job traumatic injury to the ear or infections.
Ventilation
- Ventilation is used in the workplace to control emissions, exposures, and chemical hazards, as well as to control temperature, humidity, and odors.
Industrial ventilation generally involves the use of supply and exhaust ventilation to control emissions, exposures, and chemical hazards in the workplace. Traditionally, nonindustrial ventilation systems commonly known as heating, ventilating, and air-conditioning (HVAC) systems were built to control temperature, humidity, and odors.
The Occupational Safety and Health Administration (OSHA) standard for industrial ventilation is found at 1910.94 — Ventilation. Specific operations are covered in separate paragraphs within the standard, including: 1910.94(a) — Abrasive blasting, 1910.94(b) — Grinding, polishing, and buffing operations, and 1910.94(c) — Spray finishing.
Several other standards also contain ventilation requirements. For example, those for welding are found in 1910.252; exposure to carcinogens is found in 1910.1003 to 1910.1016; dipping and coating is found in 1910.124; exposure to lead is found in 1910.1025; and cadmium exposure is found in 1910.1027.
Who must comply?
- Workplaces with certain specific types of operations must supply ventilation in the form of general exhaust ventilation or local exhaust ventilation, depending on the type of emission.
The Occupational Safety and Health Administration (OSHA) requirements generally apply to workplaces that have specific types of operations.
According to the OSHA Technical Manual, general exhaust ventilation (dilution ventilation) is appropriate when:
- Emission sources contain materials of relatively low hazard. (The degree of hazard is related to toxicity, dose rate, and individual susceptibility.)
- Emission sources are primarily vapors or gases, or small, respirable-size aerosols (those not likely to settle).
- Emissions occur uniformly; emissions are widely dispersed.
- Moderate climatic conditions prevail; heat is to be removed from the space by flushing it with outside air.
- Concentrations of vapors are to be reduced in an enclosure.
- Portable or mobile emission sources are to be controlled.
Local exhaust ventilating is appropriate when:
- Emission sources contain materials of relatively high hazard.
- Emitted materials are primarily larger-diameter particulates (likely to settle).
- Emissions vary over time.
- Emission sources consist of point sources.
- Employees work in the immediate vicinity of the emission source.
- The plant is located in a severe climate.
- Minimizing air turnover is necessary.
Key definitions
- Key terms for ventilation are defined in this section.
Key terms commonly used with ventilation controls are defined in this section. It’s important to understand these terms to ensure uniformity with safety plan development, communication, and development.
- Abrasive: A solid substance used in an abrasive blasting operation.
- Abrasive blasting: The forcible application of an abrasive to a surface by pneumatic pressure, hydraulic pressure, or centrifugal force.
- Abrasive-blasting respirator: A respirator constructed so that it covers the wearer’s head, neck, and shoulders to protect from rebounding abrasive.
- Abrasive cutting-off wheels: Organic-bonded wheels, the thickness of which is not more than one forty-eighth of their diameter for those up to, and including, 20 inches in diameter, and not more than one-sixtieth of their diameter for those larger than 20 inches in diameter, used for a multitude of operations variously known as cutting, cutting off, grooving, slotting, coping, and jointing, and the like. The wheels may be solid, consisting of organic-bonded abrasive material throughout; steel centered, consisting of a steel disc with a rim of organic-bonded material molded around the periphery; or of the inserted tooth type, consisting of a steel disc with organic-bonded abrasive teeth or inserts mechanically secured around the periphery.
- Blast cleaning barrel: A complete enclosure which rotates on an axis, or which has an internal moving tread to tumble the parts, in order to expose various surfaces of the parts to the action of an automatic blast spray.
- Blast cleaning room: A complete enclosure in which blasting operations are performed and where the operator works inside of the room to operate the blasting nozzle and direct the flow of the abrasive material.
- Blasting cabinet: An enclosure where the operator stands outside and operates the blasting nozzle through an opening or openings in the enclosure.
- Dust collector: A device or combination of devices for separating dust from the air handled by an exhaust ventilation system.
- Exhaust ventilation system: A system for removing contaminated air from a space, comprising two or more of the following elements: (a) enclosure or hood, (b) duct work, (c) dust collecting equipment, (d) exhauster, and (e) discharge stack.
- Minimum maintained velocity: The velocity of air movement which must be maintained in order to meet minimum specified requirements for health and safety.
- Particulate-filter respirator: An air purifying respirator, commonly referred to as a dust or a fume respirator, which removes most of the dust or fume from the air passing through the device.
- Polishing and buffing wheels: All power-driven rotatable wheels composed all or in part of textile fabrics, wood, felt, leather, or paper, that may be coated with abrasives on the periphery of the wheel for purposes of polishing, buffing, and light grinding.
- Respirable dust: Airborne dust in sizes capable of passing through the upper respiratory system to reach the lower lung passages.
- Rotary blast cleaning table: An enclosure where the pieces to be cleaned are positioned on a rotating table and are passed automatically through a series of blast sprays.
- Scratch brush wheels: All power-driven rotatable wheels made from wire or bristles and used for scratch cleaning and brushing purposes.
- Spray-finishing operations: The employment of methods wherein organic or inorganic materials are used in dispersed form for deposit on surfaces to be coated, treated, or cleaned. Such methods of deposit may involve either automatic, manual, or electrostatic deposition but do not include metal spraying or metallizing, dipping, flow coating, roller coating, tumbling, centrifuging, or spray washing and degreasing as conducted in self-contained washing and degreasing machines or systems.
- Spray booths: Defined and described in 1910.107(a).
- Spray room: A room in which spray-finishing operations not conducted in a spray booth are performed separately from other areas.
General workplace ventilation requirements
- Engineering control techniques such as isolation and substitution can reduce chemical exposure.
Perhaps the most widely used technique for controlling chemical exposure is the use of ventilation. General ventilation uses the movement of air within the general workspace to displace or dilute contaminants with fresh outside air.
However, general ventilation may not be the preferred control method due to the large volumes of air movement it requires. Local exhaust ventilation uses a much smaller volume of air and controls emissions at the point the contaminants are generated. Isolation and substitution controls should also be considered while creating a workplace or containment ventilation plan.
Isolation
Isolation involves placing a physical barrier between the hazardous operation and the worker. Many modern, automated manufacturing processes are fully enclosed in ventilated cabinets. The effectiveness of such a control technique depends on how frequently the workers have to enter the enclosure during normal operations.
In other situations, the worker, rather than the process or machine, can be placed in an enclosure having a controlled atmosphere. Many processes that involve potential chemical exposures are operated remotely by workers in air-conditioned booths isolated from the hazardous materials.
Substitution
Substitution refers to the replacement of a toxic chemical in a particular process or work area with a less toxic or non-toxic product. Properly applied, substitution can be a very effective control technique.
However, the proposed substitute must be carefully evaluated before use to ensure:
- That it performs in a similar manner to the product being replaced,
- That it doesn’t inadvertently introduce another hazard, and
- That it is compatible with existing manufacturing equipment and processes.
The success of these engineering control techniques will depend on the physical properties of the chemicals and emissions encountered (boiling point, vapor pressure, etc.) and the process operating conditions. In some cases, particularly with cleaning solvents, substitution may provide the quickest and most effective means of reducing exposure. In other situations, a major effort may be required to alter processes or install or expand local or general dilution ventilation.
According to the Occupational Safety & Health Administration (OSHA), engineering controls and improved work practices are able to reduce exposure levels to the required levels in almost all circumstances. However, respiratory protection may be necessary to complement engineering controls in some circumstances and to achieve compliance in specific operations in some industries.
Industry and work activity requirements
- Some industries and work activities, such as construction, have specific ventilation requirements.
Certain industries and work activities have specific ventilation requirements that employers must follow. These requirements generally involve using supply and exhaust ventilation to control emissions, exposures, and chemical hazards in the workplace. (These functions are distinct from those of nonindustrial ventilation systems known as heating, ventilating, and air-conditioning [HVAC] systems, which primarily control temperature, humidity, and odors.)
Most ventilation requirements are the same for general industry and construction.
General industry
The Occupational Safety & Health Administration (OSHA) general industry standard for ventilation is found at 1910.94. General industry employers must:
- Assess the workplace for any operations that have ventilation requirements, e.g., abrasive blasting, buffing, spray finishing, and welding.
- Provide appropriate ventilation systems.
- Maintain ventilation systems.
Construction
The ventilation standard for construction is found at 1926.57.
Specific to the industry are the requirements for open-surface tank operations. All employees working in and around such operations must be instructed on the job’s hazards and the applicable personal protection and first aid procedures.
When it’s necessary for an employee to enter a tank that may contain a hazardous atmosphere, a trained stand-by employee with a suitable respirator must also be present.
Work activity requirements
- Certain work activities — especially dipping, coating, welding, and cutting — have significant and specific ventilation hazards, with corresponding requirements.
Some work activities require more ventilation than others. In particular, workers who are involved in dipping and coating processes and in welding and cutting processes are at risk from a variety of airborne substances.
Dipping and coating
Dipping and coating pose inhalation and fire hazards due to the liquids used in these processes. Employers are responsible for controlling these hazards as much as possible and providing workers with appropriate protection.
When a liquid in a dip tank creates an exposure hazard covered by a standard listed in 1910 Subpart Z, worker exposure must be controlled as required by that standard.
The ventilation provided in a vapor area must keep the airborne concentration of any substance below 25 percent of its lower flammable limit (LFL). Employers must have a system that sounds an alarm and automatically shuts down the operation when the vapor concentration for any substance in the exhaust airstream exceeds 25 percent of its LFL.
Exhaust air may not be recirculated when any substance in that air poses a health hazard to employees or exceeds 25 percent of its LFL. The employer must ensure that any exhaust air recirculated from a dipping or coating operation using flammable liquids or liquids with flashpoints greater than 199.4°F (93°C) is:
- Free of any solid particulate that poses a health or safety hazard for employees; and
- Monitored by approved equipment.
When mechanical ventilation is used, each dip tank must have an independent exhaust system unless the combination of substances being removed will not cause a fire, explosion, or chemical reaction. Mechanical ventilation must draw the flow of air into a hood or exhaust duct.
Any mechanical ventilation used must conform to the following standards that are incorporated by reference as specified in 1910.6:
A tank cover or material that floats on the surface of the liquid in a dip tank may be used to replace or supplement ventilation. The method or combination of methods used must maintain the airborne concentration of the hazardous material and the workers’ exposure within the limits specified in paragraphs (b)(1) and (b)(2) of 1910.124.
Welding and cutting
Welders can be exposed to a number of fumes, gases, and dusts. These contaminants can harm the health of workers and accumulate to the point of causing a fire. Ventilation can help to reduce their concentration.
According to the Occupational Safety and Health Administration (OSHA), whenever and wherever welding, also known as “hot work,” occurs, everyone involved in the operation must be aware of welding fumes and gases and take necessary, especially ventilation, precautions.
Welding ventilation techniques vary. Often, however, a relatively simple ventilation method like the appropriate use of fans is all that is needed. OSHA’s standard at 1910.252(c) specifies that if mechanical ventilation is used, it must consist of either:
- General mechanical ventilation, or
- A local exhaust system.
Mechanical ventilation changes the air. In contrast, local exhaust systems, like hoods at the arc and fans, remove fumes and smoke at the source. Both ventilation methods help to reduce the concentration of hazardous fumes and gases.
Ventilation also prevents the accumulation of flammable gases, vapors, and dusts that could cause fire. Open spaces, too, can help reduce accumulations.
When ventilation doesn’t give enough protection or when welding creates an oxygen-deficient area, workers should wear respirators. Workers should also be trained not to get too close to the fume or gas plume. They should know the symptoms of overexposure to fumes and gases and leave the area if symptoms develop.
Confined spaces can pose additional fume and gas hazards because welding fumes and gases can displace oxygen or fill a confined space. Flammable or combustible fumes and gases can accumulate and cause fire, explosion, and asphyxiation. For these reasons, employers should evaluate the atmospheres of the confined space for hazards and use ventilation and respirators properly.
Because many toxic gases and vapors on the job cannot be smelled or seen, atmospheric testing and monitoring is very important. Generally, if a space has a hazardous atmosphere, the hazard must be eliminated or reduced by:
- Purging the hazardous atmosphere,
- Displacing the noncombustible gas,
- Flushing the hazardous atmosphere, and/or
- Ventilating with forced air.
For more information about welding and cutting, see Welding and Cutting.
- Under OSHA’s General Duty Clause, employers are responsible for controlling pollutants indoors to provide a safe workplace for employees.
Indoor air quality (IAQ) refers to the air quality within and around buildings and structures, especially as it relates to the health and comfort of building occupants. Understanding and controlling common pollutants indoors can help reduce the risk of indoor health concerns.
The Occupational Safety and Health Administration (OSHA) does not have a specific standard to regulate IAQ. However, employers must follow the General Duty Clause of the OSH (Occupational Safety and Health) Act, which requires them to provide workers with a safe workplace that does not have any known hazards that cause or are likely to cause death or serious injury, even when there is not an OSHA standard that applies.
Therefore, employers should be reasonably aware of the possible sources of poor IAQ, and they should have the resources necessary to recognize and control workplace hazards. It is also employers’ responsibility to inform employees of the immediate dangers that are present. Specific state and local regulations also may apply.
The two main causes of IAQ problems are indoor pollution sources and improper ventilation. Some common pollutants found in the workplace include:
- Tobacco smoke,
- Asbestos,
- Formaldehyde,
- Cleaning agents,
- Air fresheners,
- Mold,
- Radon,
- Carbon monoxide,
- Paints,
- Pesticides, and
- Adhesives.
Inadequate ventilation can increase indoor pollutant levels by not bringing in sufficient outside air to dilute emissions from indoor sources, and by not carrying indoor pollutants outside of the facility. High temperatures and humidity levels can also increase concentrations of certain pollutants.
In addition, poorly located vents can even pull in outdoor air pollutants such as diesel exhaust, boiler emissions, or fumes from dumpsters. Dirty ventilation systems can harbor biological indoor air pollutants such as molds, germs, and other contaminants, and they can circulate dirt and soot throughout the workplace.
Key definitions
- Key terms for indoor air quality are defined in this section.
Key terms commonly used in relation to indoor air quality are defined in this section. It’s important to understand these terms to ensure uniformity with safety plan development, communication, and development.
- Building-related illness (BRI): A specific illness that has been diagnosed and attributed directly to airborne building contaminants.
- Indoor air quality (IAQ): The air quality within and around buildings and structures.
- Secondhand smoke: The smoke inhaled involuntarily by people around a smoker.
- Sick building syndrome: Any number of symptoms or illnesses that are caused by exposures to unidentified contaminants in indoor air.
- Volatile organic compounds (VOCs): Organic chemical compounds whose composition makes it possible for them to evaporate under normal indoor atmospheric conditions of temperature and pressure.
General indoor air quality information
- Factors affecting indoor air quality include temperature, humidity, ventilation, and the presence and concentration of inside and outside pollutants.
Indoor air quality (IAQ), also called indoor environmental quality, describes how inside air can affect people’s health, comfort, and ability to work. It can include temperature, humidity, poor ventilation, mold from water damage, and exposure to other chemicals. Currently, the Occupational Safety and Health Administration (OSHA) has no IAQ standards.
The qualities of good IAQ include:
- Comfortable temperature and humidity,
- An adequate supply of fresh outdoor air, and
- Control of pollutants from inside and outside of the building.
Causes of IAQ problems
The most common causes of IAQ problems in buildings are:
- Inadequate ventilation;
- Lack of fresh outdoor air;
- Contaminated air being brought into the building;
- Poor upkeep of ventilation, heating, and air-conditioning systems;
- Dampness and moisture damage due to leaks, flooding, or high humidity;
- Construction or remodeling activities; and
- Contaminated air.
The National Institute for Occupational Safety and Health (NIOSH) found that microbial contamination and contamination from building fabric are also significant sources of IAQ problems.
The relative importance of any single source depends on how much of a given pollutant it emits and how hazardous those emissions are. In some cases, factors such as how old the source is and whether it is properly maintained are significant. For example, an improperly adjusted gas stove can emit significantly more carbon monoxide than one that is properly adjusted.
Also, inadequate ventilation can increase indoor pollutant levels by not bringing in enough outdoor air to dilute emissions from indoor sources and by not carrying indoor air pollutants out of the building. High temperature and humidity levels can also increase concentrations of some pollutants.
Some sources, such as building materials, furnishings, and household products like air fresheners, release pollutants more or less continuously. Other sources, related to activities carried out in the building, release pollutants intermittently. These include:
- Smoking;
- The use of unvented or malfunctioning stoves, furnaces, or space heaters;
- The use of solvents in cleaning and hobby activities;
- The use of paint strippers in redecorating activities; and
- The use of cleaning products and pesticides in housekeeping.
Whether released continuously or intermittently, high concentrations of pollutants can remain in the air for long periods.
Although OSHA has no specific IAQ requirements for employers, poor IAQ is hazardous to employees. Therefore, maintaining good IAQ is employers’ responsibility under the General Duty Clause.
At the most basic, employers must:
- Conduct an assessment of the facility’s indoor air quality.
- If need be, hire an industrial hygienist or other professional to take measurements and offer recommendations.
- Locate dumpsters, smoking areas, chemical storage, and other sources of odors or emissions away from building air intakes.
Identifying indoor air quality problems
- There is no single test for IAQ problems, but they can often be identified by inspecting the workplace and gathering information about symptoms suffered by employees.
Buildings with poor indoor air quality (IAQ) may have unpleasant or musty odors or feel hot and stuffy. Some workers may complain about symptoms that happen at work and go away when they leave work, like having headaches or feeling tired. Fever, cough, and shortness of breath among employees can be symptoms of a more serious problem.
However, not all exposures cause symptoms, so there is no substitute for good building management.
Inspecting for IAQ problems
There is no single test to find an IAQ problem. Regular inspections and testing should be done, checking:
- Temperature, humidity, and airflow;
- Whether the ventilation, heating, and air conditioning systems are working according to specifications for building use and occupancy; and
- Whether odors, water damage, leaks, dirt, or pest droppings are present.
Sources that may lead to IAQ problems need to be eliminated. Standing water in humidifiers, air conditioning units, on roofs, and in boiler pans can become contaminated with bacteria or fungi. In some circumstances, specific testing for radon or for asbestos may be required as part of building occupancy.
Assessing employee symptoms
It is often difficult to determine if symptoms are a result of exposure to poor IAQ or some other factors. However, the following questions may be helpful in figuring out if there is an IAQ problem at a facility:
- Do employees have symptoms that just occur at work and go away when they get home?
- What are these symptoms?
- Are these symptoms related to a certain time of day, a certain season, or certain location in the workplace?
- Did the symptoms start when something new happened in the workplace, such as renovation or construction projects?
- Are there other employees at work with similar complaints?
- Did any employee see a doctor for the symptoms, and if so, did the doctor diagnose an illness related to IAQ?
If answers to the above questions indicate a possible IAQ issue, an effort should be made to identify indoor air sources at the worksite that may be possible causes.
Health impacts of indoor air quality
- Indoor air pollutants can cause both immediate symptoms and later illness.
- Building-related illnesses are those that are linked to specific building problems.
Modern buildings are generally considered safe and healthful work environments. However, energy conservation measures instituted during the early 1970s have minimized the infiltration of outside air and contributed to the buildup of indoor air contaminants.
Health effects from indoor air pollutants fall into two categories:
- Those that are experienced immediately after exposure, and
- Those that do not show up until later.
Immediate effects, which may show up after a single exposure or repeated exposures, include:
- Irritation of the eyes, nose, and throat;
- Headaches;
- Dizziness; and
- Fatigue.
Immediate effects are usually short-term and treatable. Sometimes, the prescribed treatment is to simply eliminate the person’s exposure to the source of the pollution, if it can be identified. Symptoms of some diseases, such as asthma, can show up soon after exposure to some indoor air pollutants.
The likelihood of an individual developing immediate reactions to indoor air pollutants depends on several factors, such as age and pre-existing medical conditions. In other cases, whether a person reacts to a pollutant can be determined by individual sensitivity, which varies from person to person.
Other health effects may show up either years after the exposure has occurred, or only after long or repeated periods of exposure. The consequences of these types of exposures can include respiratory diseases, heart disease, and cancer.
While pollutants commonly found in indoor air can be responsible for many harmful effects, there is considerable uncertainty about what concentrations or periods of exposure are necessary to produce specific adverse health effects. Further research is needed to better understand which health effects can occur after exposure to low-level pollutant concentrations, as well as higher-level concentrations.
Building-related illnesses
A number of well-identified illnesses, such as Legionnaires’ disease, asthma, hypersensitivity, pneumonitis, and humidifier fever, have been directly traced to specific building problems. These are called building-related illnesses. Most of these diseases can be treated; nevertheless, some pose serious risks.
Sometimes, however, building occupants experience symptoms that do not fit the pattern of any particular illness and are difficult to trace to any specific source. This phenomenon has been labeled “sick building syndrome.” People may complain of one or more of the following symptoms:
- Dry or burning mucous membranes in the nose, eyes, and throat;
- Sneezing;
- Stuffy or runny nose;
- Fatigue or lethargy;
- Headache;
- Dizziness;
- Nausea;
- Irritability; and
- Forgetfulness.
Poor lighting, noise, vibration, thermal discomfort, and psychological stress may also cause, or contribute to, these symptoms.
There is no single manner in which these symptoms appear. In some cases, problems begin as workers enter the building and diminish as they leave; other times, symptoms continue until the illness is treated. Sometimes there are outbreaks of illness among many workers in a single building; in other cases, health symptoms show up only in individual workers.
Multiple chemical sensitivity
- Multiple chemical sensitivity involves sensitivity to low concentrations of various chemicals; however, its existence has not been scientifically confirmed.
Multiple chemical sensitivity (MCS) refers to a condition in which a person is considered to be sensitive to a number of chemicals at very low concentrations. It is often discussed in relation to indoor air quality (IAQ).
Symptoms of MCS involve more than one organ and seem to be brought on by exposure to very low levels of chemicals. Some symptoms include fatigue, loss of concentration, depression, and joint and muscle pain. However, no physical signs have been found consistently in MCS patients.
Stimuli that are believed to bring on the effects include pesticides, paints, adhesives, carpets and carpet cleaning materials, fragrances in perfumes and personal hygiene products, molds and fungi, petroleum products, electromagnetic fields, dental fillings, trauma, and industrial chemicals. Odors are often thought to be triggers.
Employers are responsible for helping employees who complain about symptoms that seem to come from the air. They have to find ways to accommodate complainants and work with them to help alleviate the symptoms.
MCS may affect a small percentage of the population and is not currently recognized by the major medical organizations. Medical opinion is divided, however, and further research is needed.
Proposed theories to explain the cause of MCS include allergy, dysfunction of the immune system, neurobiological sensitization, and various psychological theories. There is insufficient scientific evidence to confirm a relationship between any of these possible causes and symptoms. Due to the lack of definite information, an evaluation must be performed by a physician knowledgeable of the symptoms of this condition.
Lighting in the workplace
- Poor workplace lighting can lead to injury in the workplace, as well as inefficiency due to difficulty operating equipment.
Poor workplace lighting can lead to slips, trips, and falls, as well as inability to exit a space safely, difficulty operating equipment, and a host of other hazards. Workplace lighting must take into account quantity, quality, direction and a number of other factors to ensure safety. In addition, lighting types can cause problems themselves, for example, some types take a while to warm up and some types impact appearance of colors, which can lead to inability to recognize safety signs, for example.
Lighting — General industry
- OSHA does not usually specify the amount of illumination required in the workplace, although there are other standards that indicate recommended levels depending on the environment and work being done.
The Occupational Health and Safety Administration (OSHA)’s general industry regulations, for the most part, do not go into specifics about the amount of illumination required. OSHA’s Powered Industrial Truck standard is one of the few places that a specific illumination level is given. Paragraph 1910.178(h)(2) states, “Where general lighting is less than 2 lumens per square foot, auxiliary directional lighting shall be provided on the truck.” OSHA also addresses adequate lighting in the exit routes rule at 1910.37(b).
There is an American National Standards Institute (ANSI) standard for industrial lighting that is incorporated by reference (ANSI A11.1-65 — Practice for Industrial Lighting) in the OSHA standards for mechanical power-transmission apparatus (1910.219(c)(5)(iii)), pulp and paper mills (1910.261(a)(3)), and sawmills (1910.265(c)(2)).
In general, OSHA uses the General Duty Clause of the OSH Act to cite most hazards related to poorly-lit workplaces, often referencing the ANSI standard (which is now replaced by the Illuminating Engineering Society of North America (IESNA) RP-7: Recommended Practice for Lighting Industrial Facilities).
This industry standard provides recommended levels based on the type of work being done and the environment. Lighting needs vary depending on such things as amount of activity, hazard of the environment, and other factors, generally ranging from .5 foot-candles for low hazard areas (e.g., offices) to 5.0 for high hazards and activity levels (such as machine shops or engine rooms). Lighting can be either artificial or natural.
Lighting — Construction
- For the construction industry, OSHA sets minimum illumination standards for certain locations such as general construction areas, warehouses, corridors, exits, tunnels and underground work areas, and more.
The Occupational Safety and Health Administration (OSHA) requires in 1926.56(a) that construction areas, ramps, runways, corridors, offices, shops, and storage areas shall be lighted to not less than the minimum illumination intensities listed in Table D-3 while any work is in progress:
Table D-3—Minimum Illumination Intensities in Foot-Candles
| Foot-candles | Area or Operation |
|---|
| 5 | General construction area lighting. |
| 3 | General construction areas, concrete placement, excavation and waste areas, accessways, active storage areas, loading platforms, refueling, and field maintenance areas. |
| 5 | Indoors: warehouses, corridors, hallways, and exitways. |
| 5 | Tunnels, shafts, and general underground work areas: (Exception: minimum of 10 foot-candles is required at tunnel and shaft heading during drilling, mucking, and scaling. Bureau of Mines approved cap lights shall be acceptable for use in the tunnel heading.) |
| 10 | General construction plant and shops (e.g., batch plants, screening plants, mechanical and electrical equipment rooms, carpenter shops, rigging lofts and active storerooms, barracks or living quarters, locker or dressing rooms, mess halls, and indoor toilets and workrooms.) |
| 30 | First aid stations, infirmaries, and offices. |
Other areas. For areas or operations not covered above, employers should refer to the
American National Standard A11.1-1965, R1970, Practice for Industrial Lighting, for recommended values of illumination (which is now superseded by the Illuminating Engineering Society of North America (IESNA) RP-7: Recommended Practice for Lighting Industrial Facilities).